Coronavirus vaccination programmes are starting all over the world, following the approval of the Pfizer-BioNTech vaccine; Moderna’s vaccine is also likely to be approved within days.
Mass vaccination programmes are complicated logistical feats. The right amount of vaccine needs to be delivered to the right places at the right times, stored (the Pfizer vaccine needs to be kept at -70C, a crazy low temperature) and injected into people. That also means health systems need syringes, needles and nurses to do the actual injecting.
It also means deciding who gets vaccinated first. For the next few months, vaccine supplies are going to be limited as every country scrambles to buy up what they can.
Personally, I’d love to get my vaccine right now. But at the individual level, a vaccine wouldn’t change my life very much.
We know that vaccines protect against coronavirus disease – CoViD-19. But it’s possible that vaccinated people can still catch, carry and transmit the actual virus to other people, without experiencing any disease symptoms.
There’s good reason to think that vaccines DO reduce coronavirus infection and transmission, too, but that hasn’t been properly studied yet, and the reduction is likely to be less than the claimed 95% effectiveness these vaccines show at preventing disease.
So how long will it be before I can benefit from the vaccine, if it might be months before I get my turn for a jab?
Actually, the benefits will come a lot faster. Because Covid-19 is so much more risky for older people, a little vaccination goes a long way.
(The following methodology and analysis is based on Harry Lambert’s article in the New Statesman which applied it to the UK)
Three thousand Israelis have died from Covid-19. Of the casualties, 54% were over 80 years old. 80% were over 70, and 93% were over the age of 60.
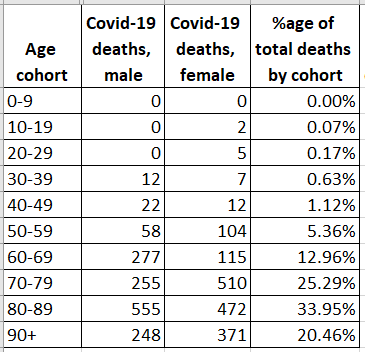
This is even more striking when considering the size of each age cohort. Israel’s young population means that the over-60s only represent 16% of the total population.
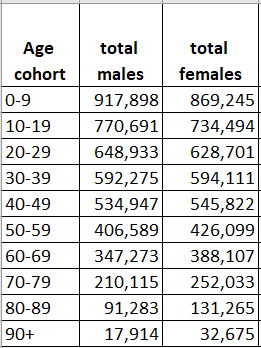
Let’s assume the vaccine is 95% effective at preventing death from Covid-19. In reality it might be higher than this, because it seems like the 5% vaccinated people who do get Covid-19 have less severe symptoms, but it’s a reasonable assumption.
With just the 51,000 over-90s vaccinated, which is around 0.5% of Israel’s population, the total risk of fatalities from Covid-19 drops a huge 19%.
Expanding vaccination to all over-80s would only require 273k people to be vaccinated, but would more than half the fatality risk of the virus.
By the time we’ve vaccinated all over-70s, we’ll be up to 76% lower fatality risk with just 735,000 people vaccinated.
For those people who are into 80-20 principles, the graph suggests that when Israel has vaccinated the most vulnerable 20% of people, the fatality risk will be reduced by 80%.
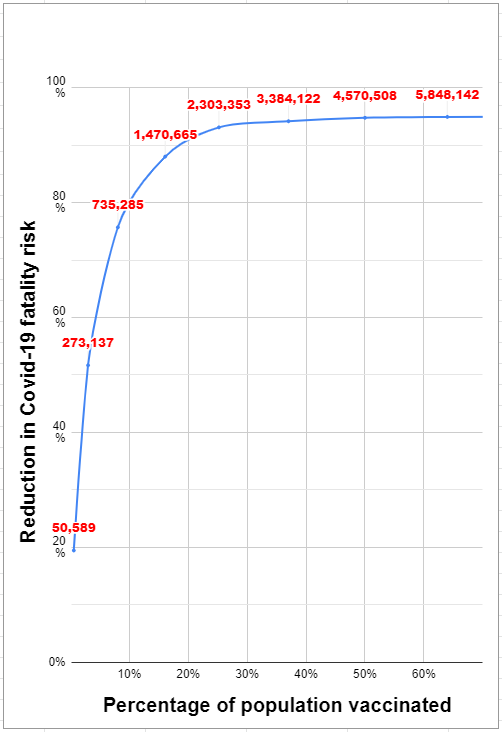
Alongside this drop in fatality should also be a drop in serious cases and hospitalisations, reducing strain on the health system as a whole.
Adding on all over-60s drops the fatality risk by 88%; adding in under-50s brings us to a 93% decrease with a quarter of the whole population vaccinated.
But from then on, vaccinating all the under-50s, which is the remaining three quarters of the population (6.8 million people), only moves the fatality risk from 93% to the maximum of 95%. And even this is misleading; we might be able to get close to 95% by targeting vaccines at vulnerable under-50s with known conditions.
So the most devastating phase of the Covid-19 pandemic is nearly over. But what comes next?
Does Israel reopen rapidly once all the over-60s are vaccinated? Reducing the risk by 93% is huge, but with unmitigated virus spread, the remaining 7% might still represent many thousands of deaths.
Equally, maintaining restrictions after mass vaccination seems crazy; isn’t the whole point that we want to get back to normal life?
My best guess is that it’s somewhere in the middle. Once the most vulnerable part of the population has been vaccinated, we’ll be able to take many more steps back towards normal life, while maintaining some restrictions.
What I’m less sure about is how that works. It’s tempting to just allow massive coronavirus spread in, say, under-40s as a path to herd immunity once all over-60s are protected. That approach could lead to thousands of deaths… but maybe they’d be in the ballpark range of annual flu, or a little higher.
Or perhaps we keep a constant level of restrictions until the whole population is vaccinated, including the 75% of us that are under 50, and hope that the vaccine also significantly reduces the risk of spreading the infection. This is a longer path back to normality, but a safer one. There’s good reason to think a vaccine will give better, stronger immunity than an asymptomatic virus case, so this is a more durable path too.
The coronavirus isn’t going away. It probably never will. But a little vaccination goes a long way to reducing the risk. Vaccinating just half a percent of Israel’s population should cut the fatality risk significantly, and just 3% will half it. There’s a lot to be hopeful about right now.
Great article. Although you never mentioned if you thought people would or wouldn’t get themselves vaccinated. I feel many don’t see themselves as anti vaxers , just want to wait see what happens to thoses who get vaccinated first? What’s your opinion on this?
I think it’s early days. Most of the vaccine scepticism is in the millennial and GenX demographics, and it will be a while before we have any space vaccines to give them anyway!
Interesting and encouraging analysis. But at one point you say that 16% of the population are over 60 and later on that 75% are under 60 …. that doesn’t quite add up.
Thanks, it should have read “75% of us that are under 50” and has now been corrected.
That is an interesting thought. In Canada we are doing healthcare workers, people in Longterm care homes and aboriginals in isolated communities that have outbreaks first.
Its a great analysis. Since the tradeoff is between fatality rates and working (economy), it will be worthwhile to study this as a percentage of working population in each cohort. I guess none of the people over 90 go to work (low transmission). But people in the 60’s go (so more transmission)
You assume of course that the immune response is the And vaccine efficacy is the same in older as in younger groups.
Yes, but I also assume that the 5% of older people who get the virus are just as likely to get serious symptoms and die, which is probably also not correct, so hopefully both assumptions roughly cancel out.
Hi Arieh, more articles related? I found it quite interesting! Thanks
Very interesting post. I would add that if there is an effect on transmission, we can use the vaccines we have to gain the most ground with that, too. For example, after vaccinating the 20% most at risk, we can move onto groups which are most likely to transmit. While restrictions are in place, vaccinating essential workers is likely to drag transmission down far lower than vaccinating people who are working from home anyway. Not sure the cost/benefit gradient would be quite as steep for this as it is for mortality, but you could maximise the effect to some extent anyway.
I think this one is complicated. If the vaccine does significantly impact transmission, then working out which groups are the most likely to transmit isn’t simple. For example, delivery drivers are essential, but maybe they don’t come into contact with many people. Schoolkids are at no real risk, but maybe they transmit a lot — but that’s still disputed… it will depend on how well we understand transmission mechanics, aerosol v droplets etc. Overall I agree, though.